Muscle overload is the main cause of hamstring muscle strain. This can happen when the muscle is stretched beyond its capacity or challenged with a sudden load.
Hamstring muscle strains often occur when the muscle lengthens as it contracts, or shortens. Although it sounds contradictory, this happens when you extend a muscle while it is weighted, or loaded. This is called an "eccentric contraction."
During sprinting, the hamstring muscles contract eccentrically as the back leg is straightened and the toes are used to push off and move forward. The hamstring muscles are not only lengthened at this point in the stride, but they are also loaded — with body weight as well as the force required for forward motion.
Like strains, hamstring tendon avulsions are also caused by large, sudden loads.
Risk Factors
Several factors can make it more likely you will have a muscle strain, including:
Muscle tightness
Tight muscles are vulnerable to strain. Athletes should follow a year-round program of daily stretching exercises.
Muscle imbalance.
When one muscle group is much stronger than its opposing muscle group, the imbalance can lead to a strain. This frequently happens with the hamstring muscles. The quadriceps muscles at the front of the thigh are usually more powerful. During high-speed activities, the hamstring may become fatigued faster than the quadriceps. This fatigue can lead to a strain.
Poor conditioning
If your muscles are weak, they are less able to cope with the stress of exercise and are more likely to be injured.
Muscle fatigue
Fatigue reduces the energy-absorbing capabilities of muscle, making them more susceptible to injury.
Choice of activity
Anyone can experience hamstring strain, but those especially at risk are:
- Athletes who participate in sports like football, soccer, basketball
- Runners or sprinters
- Dancers
- Older athletes whose exercise program is primarily walking
- Adolescent athletes who are still growing
Imaging Tests
X-rays. An X-ray can show whether you have a hamstring tendon avulsion - when the injured tendon has pulled away a small piece of bone.
Magnetic Resonance Imaging (MRI). This study can create better images of soft tissues like the hamstring muscles to ascertain if the tendon is thickened/inflamed (tendinosis) versus torn and to what extent. Muscle belly or musculotendinous injuries can also be detected.
Treatment
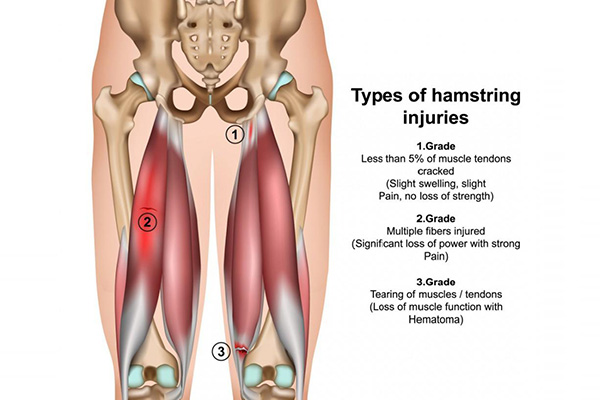
Treatment of hamstring strains will vary depending on the type of injury you have, its severity, and your own needs and expectations.
Nonsurgical Treatment
Most hamstring injuries are managed well without surgery.
RICE. The RICE protocol is effective for most sports-related injuries.
- Rest. Take a break from the activity that caused the strain.
- Ice. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly to the skin.
- Compression. To prevent additional swelling and blood loss, you may wear an elastic compression/ACE bandage, although this is best in muscle belly injuries.
- Elevation. To reduce swelling, recline and put your leg up higher than your heart while resting.
Physical therapy. Once the initial pain and swelling has settled down, physical therapy can begin. Specific exercises can restore range of motion and strength. PRP is often used as an adjunct to PT to assist with healing.
Surgical Treatment
Surgery is most often performed for tendon avulsion injuries, where the tendon has pulled completely away from the bone in the setting of those in need of return to explosive activities.
Surgery is not commonly performed for tears within the muscle belly.
Procedure. To repair a tendon avulsion, he tendon is reattached with the bone to the ischial tuberosity using anchors.
Rehabilitation. After surgery, patients will need to keep weight off of the leg to protect the repair. In addition to using crutches, a specific brace is used to reduce tension on the repair.
Rehabilitation for a proximal hamstring repair typically takes at least 6 months, due to the severity of the injury. Return to play testing, of course, is essential to make an appropriate determination.






