Biceps Tendon Injuries: How to Treat

What is Biceps tendinitis?
Biceps tendinitis is inflammation of the upper part of the biceps tendon, where it connects at the shoulder joint.
Common signs and symptoms include pain in the front of the shoulder and weakness.
Anatomy
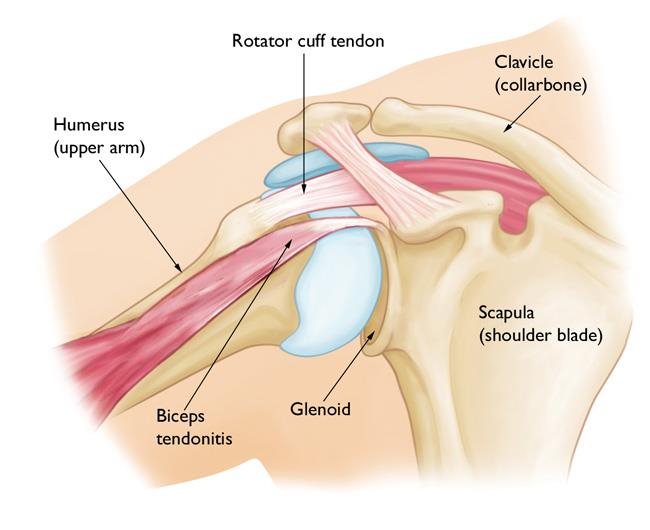
Your shoulder is a ball-and-socket joint made up of three bones: the upper arm bone (humerus), shoulder blade (scapula), and collarbone (clavicle).
Glenoid. The head of your upper arm bone (humerus) fits into the rounded socket in your shoulder blade. This socket is called the glenoid. The glenoid is lined with soft cartilage called the labrum. This tissue helps the head of the upper arm bone fit into the shoulder socket.
Rotator cuff. A combination of muscles and tendons keeps your arm centered in your shoulder socket. These tissues, called the rotator cuff, cover the head of your upper arm bone and attach it to your shoulder blade.
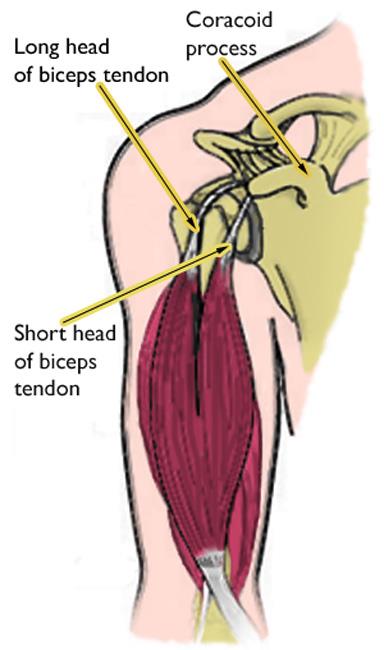
Biceps tendons. The biceps muscle is in the front of your upper arm. It has two tendons that attach it to the shoulder blade bone. The long head attaches to the top of the shoulder socket (glenoid). The short head attaches to a bump on the shoulder blade called the coracoid process.
Description
Biceps tendinitis is inflammation of the long head of the biceps tendon. In its early stages, the tendon becomes inflamedand swollen. As tendinitis develops, the tendon sheath (covering) can thicken. The tendon itself often thickens or grows larger.
The tendon in the late stages is often dark red in color due to the inflammation. Occasionally, the damage to the tendon can result in a partial or complete tear,. A complete tendon tear results in a deformity of the arm (a "Popeye" bulge in the upper arm).
Biceps tendinitis usually occurs along with other shoulder problems. In most cases, there is also damage to the rotator cuff tendons. Other problems that often accompany biceps tendinitis include:
- Arthritis of the shoulder joint
- Tears in the glenoid labrum
- Chronic shoulder instability (dislocation)
- Shoulder impingement
- Other diseases that cause inflammation of the shoulder joint lining
Cause
In most cases, damage to the biceps tendon is due to a lifetime of normal activities. As we age, everyday wear and tear causes our tendons to slowly weaken. This degeneration can be worsened by overuse — repeating the same shoulder motions again and again.
Many jobs and routine chores can cause overuse damage. Sports — particularly those that require repetitive overhead motion, such as swimming, tennis, and baseball — can also put people at risk for biceps tendinitis.
Repetitive overhead motion may play a part in other shoulder problems that occur with biceps tendinitis. Rotator cuff tears, osteoarthritis, and chronic shoulder instability are often caused by overuse.
Symptoms
- Pain or tenderness in the front of the shoulder, which worsens with overhead lifting or activity
- Pain or achiness that moves down the upper arm bone
- An occasional snapping sound or sensation in the shoulder
Doctor Examination
Physical Examination
After discussing your symptoms and medical history, your doctor will examine your shoulder.
During the examination, your doctor will assess your shoulder for range of motion, strength, and signs of shoulder instability. In addition, they will perform specific physical examination tests to check the function of your biceps.
Imaging Tests
Tests that may help your doctor confirm your diagnosis include:
X-rays. Although they only visualize bones, X-rays may show other problems in your shoulder joint.
Magnetic resonance imaging (MRI) and ultrasound. These imaging techniques can show soft tissues like the biceps tendon in greater detail than X-rays.
Treatment
Your orthopedic surgeon will work carefully to identify any other problems in your shoulder and treat them along with your tendinitis.
DISEASES & CONDITIONS
TREATMENT
DISEASES & CONDITIONS
Nonsurgical Treatment
Biceps tendinitis is typically first treated with simple methods. This type of nonsurgical treatment is usually effective in most patients.
Rest. The first step toward recovery is to avoid activities that cause pain.
Ice. Apply cold packs for 20 minutes at a time, several times a day, to keep swelling down. Do not apply ice directly to the skin.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs like ibuprofen, aspirin, and naproxen can reduce pain and swelling.
Steroid injections. Steroids such as cortisone are very effective anti-inflammatory medicines. Injecting steroids into the tendon can relieve pain. Your doctor will use these cautiously, however. In rare circumstances, steroid injections can further weaken the already injured tendon, causing it to tear.
Physical therapy. Specific stretching and strengthening exercises can help restore range of motion and strengthen your shoulder.
Surgical Treatment
If your condition does not improve with nonsurgical treatment, your doctor may offer surgery as an option. Surgery may also be an option if you have other associated shoulder problems.
During arthroscopy, your surgeon inserts the arthroscope and small instruments into your shoulder joint.
Surgery for biceps tendinitis is usually performed arthroscopically. This allows your doctor to assess the condition of the biceps tendon as well as other structures in the shoulder.
During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your shoulder joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments.
Repair. Rarely, the biceps tendon can be repaired where it attaches to the shoulder socket (glenoid).
Biceps tenodesis. In some cases, the damaged section of the biceps is removed, and the surgeon reattches the remaining tendon to the upper arm bone (humerus). This procedure is called a biceps tenodesis. Removing the painful part of the biceps usually resolves symptoms and restores normal function.
Depending on your situation, your surgeon may choose to do this procedure arthroscopically or through an open incision.
Tenotomy. In some cases, the long head of the biceps tendon may be so damaged that it is not possible to repair or tenodese it. Your surgeon may simply elect to release the damaged biceps tendon from its attachment. This is called a biceps tenotomy. This option is the least invasive but may result in a Popeye bulge in the arm. Patients who have tenotomy usually do well and return to near normal strength.
Information courtesty of AAOS OrthoInfo